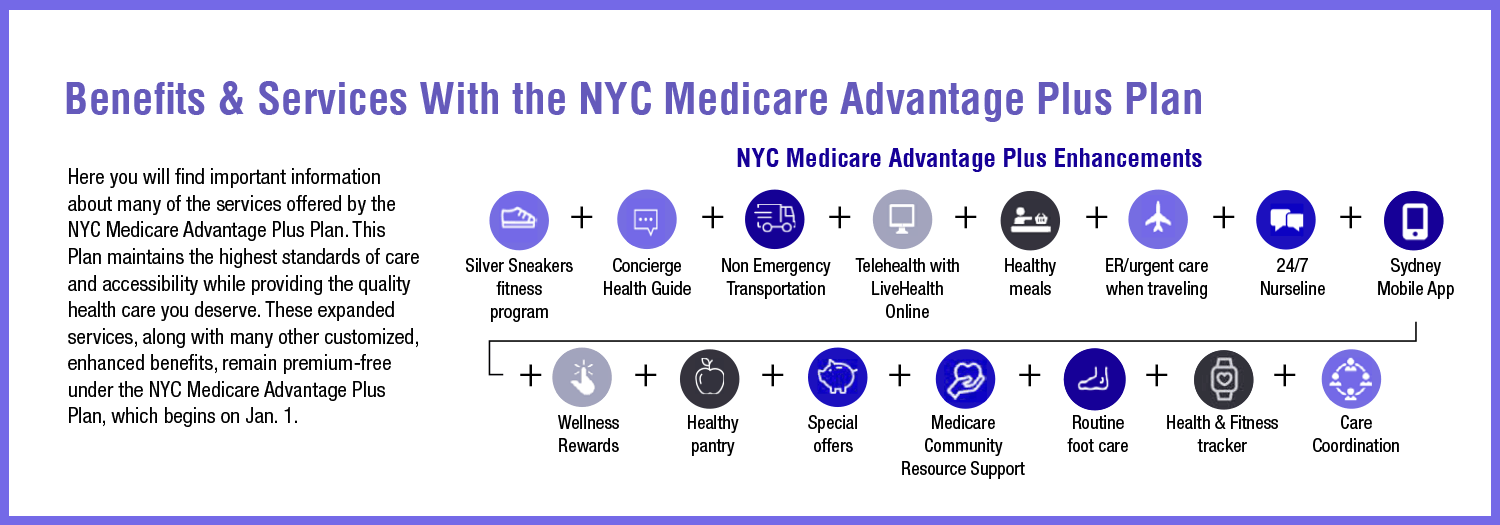
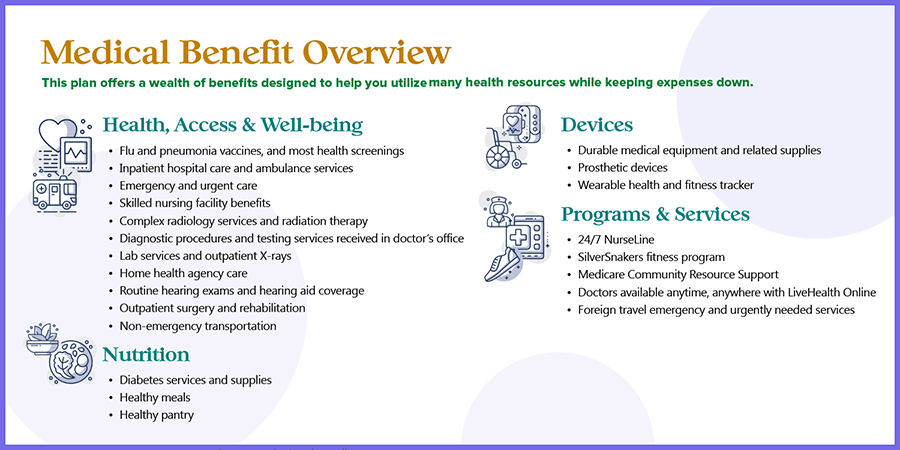
Medical Benefit Overview
This plan offers a wealth of benefits designed to help you utilize many health resources while keeping expenses down.

• Flu and pneumonia vaccines, and most health screenings
• Inpatient hospital care and ambulance services
• Emergency and urgent care
• Skilled nursing facility benefits
• Complex radiology services and radiation therapy
• Diagnostic procedures and testing services received in doctor’s office
• Lab services and outpatient X-rays
• Home health agency care
• Routine hearing exams and hearing aid coverage
• Outpatient surgery and rehabilitation
• Non-emergency transportation
• Diabetes services and supplies
• Healthy meals
• Healthy pantry
• Durable medical equipment and related supplies
• Prosthetic devices
• Wearable health and fitness tracker

• 24/7 NurseLine
• SilverSnakers fitness program
• Medicare Community Resource Support
• Doctors available anytime, anywhere with LiveHealth Online
• Foreign travel emergency and urgently needed services